Letters to the Editor is a periodical column. We welcome all comments and will post a selection. We edit for length and clarity and require full names.
Strengthen the PAs
The article Primary care interrupted: Will the doctor see you now? The Changing Landscape of Healthcare Systems (June 28) devalues a key solution critical to meeting our nations’ healthcare needs: PAs (Physician Associates/Physician Assistants).
Our country’s more than 168,300 PAs provide critical patient care in all communities, including those where physicians are unable to meet patient demand. In fact, a recent Harris Poll survey found that the majority of adults (68%) have seen a PA and nearly 6 in 10 have seen the same PA more than once. Of respondents, 93% of adults agreed that PAs add value to health care teams, and 90% said PAs increase their access to care and make it easier to get an appointment when they need it. These findings are consistent with the PA’s approach to health care: transforming health through patient-centered, team-based practice to help achieve greater health equity in underserved communities.
As the physician shortage worsens, it is imperative that legislators in states and the federal government implement policies that ensure that PAs are able to practice and provide care to the fullest extent of their education and training. The future of our nation’s healthcare system depends on the PA workforce being fully empowered to be a part of the patient-centered solution.
Lisa M. Gables, CEO of the American Academy of Physician Associates, Alexandria, Virginia
On Twitter, Ellen Andrews, executive director of the Connecticut Health Policy Project, said:
Ellen Andrews, Hamden, Connecticut
Osteopathic doctors to the rescue
I applaud the recent article As Fewer MDs Practice Rural Primary Care, a Different Type of Doctor Helps Take Up the Slack (June 6), which clearly illustrates how rural communities are facing a crisis in primary care coverage. Even before the covid-19 crisis, an additional 14,100 to 17,600 doctors were needed in non-metropolitan areas for underprivileged populations to have the same access to care as their more urban counterparts.
This unequal access to health care has real-world health implications. A study by the Centers for Disease Control and Prevention showed that rates for the top 10 causes of death were higher in rural areas than in urban areas, with the greatest difference being the rates of deaths from heart disease, cancer and chronic eye diseases. lower respiratory tract.
Fortunately, osteopathic medical education is ready and prepared to play an important role in meeting this challenge. As we celebrate its 125th anniversary this week, the American Association of Colleges of Osteopathic Medicine is proud to represent 40 colleges of osteopathic medicine (COM) in 64 teaching locations in 35 states. In fact, the number of colleges has doubled since 2000, and today more than 35,000 prospective physicians, 25% of all US medical students, are educated at our COMs. That number is projected to rise to 1 in 3 medical students by 2030.
We are also training our future doctors where patients need it most. Sixty percent of our COMs are in a federally designated healthcare professional shortage area, and 64 percent require clinical rotations in rural and underserved communities. The historical connection between the osteopathic philosophy of holistic and preventive care and primary care is making a real difference, especially in states where COMs have been training physicians for decades.
For example, according to a recent National Center for the Analysis of Healthcare Data study, since 1985 alone the Michigan State University College of Osteopathic Medicine has graduated 6,580 DOs who are still in active practice, and 73 percent of those alumni (4,776) currently practices in Michigan more than any other medical school in the state can boast. Similarly, the West Virginia School of Osteopathic Medicine has more graduates practicing in the state and more graduates practicing in rural areas than the other two medical schools in the state combined.
And there are more COMs opening in underserved rural areas like Montana, Kansas and Tennessee.
Osteopathic medicine is now firmly entrenched in the American medical system and is more sought after by both patients and prospective students than ever. Just as we have done for 125 years, AACOM and the osteopathic medical education community stand ready to work with our colleagues to overcome the health care challenges our country faces and will face.
Robert Cain, president and CEO of AACOM, Bethesda, Maryland
Elsa Pearson Sites, who serves as the policy director for the Partnered Evidence-based Policy Resource Center for the Department of Veterans Affairs at the VA Boston Healthcare System, chimed in with this tweet:
Sites of Elsa Pearson, Boston
Who is Really Responsible for Handling Opioid Liquidation Cash?
In the article Payback: Tracking Opioid Cash: Meet the People Deciding How to Spend $50 Billion in Opioid Settlement Cash (July 10), the Colorado Settlement Line says the state council controls 80 percent of the state’s transaction. While this may be technically true, this is not the case in practice.
In practice, regional councils have complete autonomy in how their money is spent within a menu of virtually all possible opioid-related spending choices. Developing this menu was part of the Colorado Opioid Abatement Councils mandate, but it is too broad to effectively limit regional spending. Thus, the COAC oversees 10% of state money and the Attorney General’s Office and Board oversees 10% of state money, but the other 60% is regional and most of the remaining 20% actually ends up in regional hands because many municipalities hand over the funds to the regional council. So these regional councils actually oversee over 70% of state funding.
It seems that, for our state, the article significantly overestimates the role of state councils. While they’re very important, they don’t actually make decisions about anywhere near 80 percent of our states’ settlement money. I wonder if there are similar situations in other states?
JK Costello, Steadman Group, Denver
A patient advocate in Washington and a podcaster in Illinois tweeted their reactions:
Janice Tufte, Seattle
Jonathan Singer, Evanston, Ill
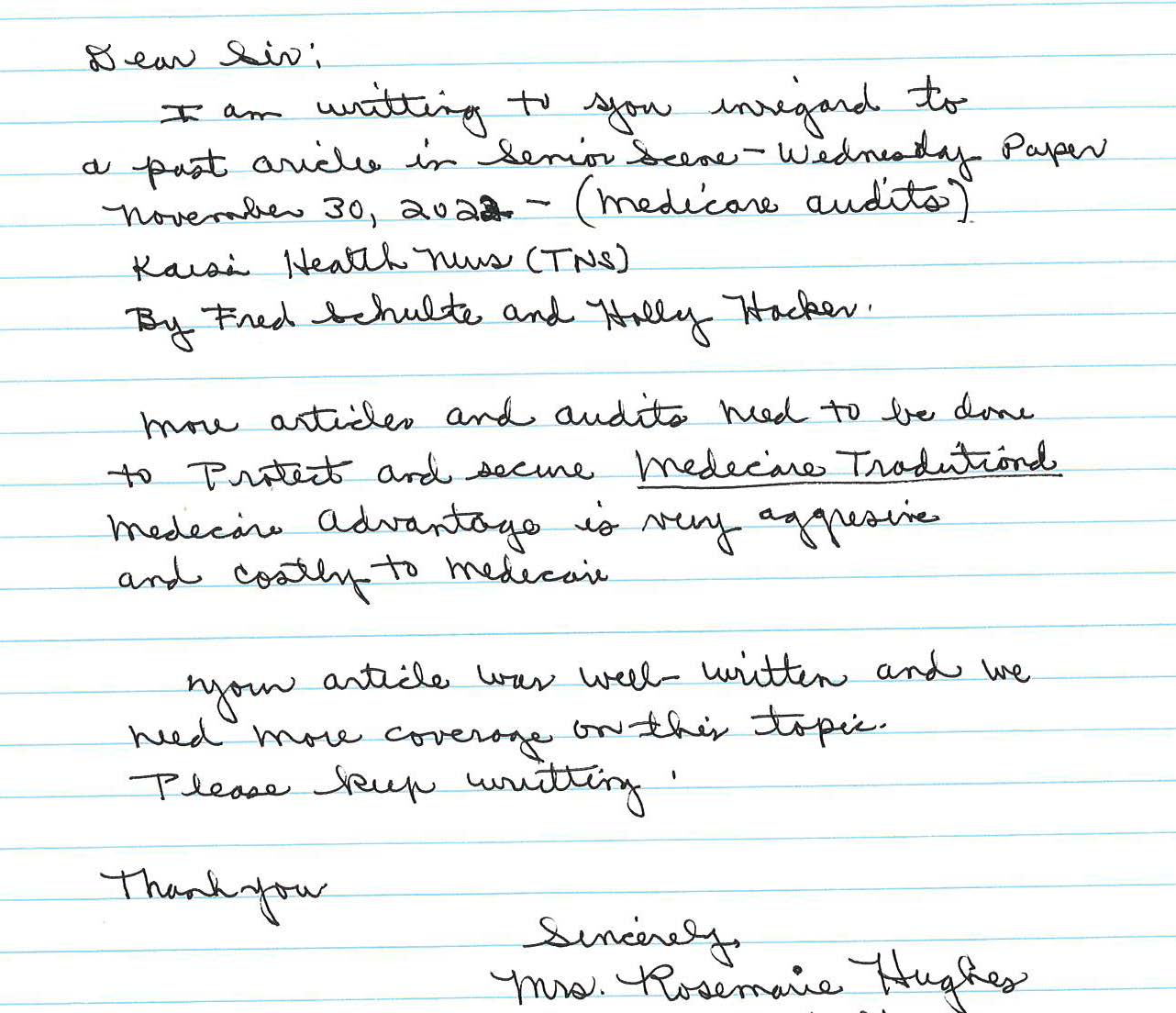
A handwritten plea to keep writing
I am writing about an earlier article in the Senior Scene paper (Audits Hidden Until Now Reveal Millions in Medicare Advantage Overcharges, Nov. 21) about Medicare audits by Fred Schulte and Holly K. Hacker.
More items and checks need to be done to protect and secure traditional Medicare. Medicare Advantage is very aggressive and expensive for Medicare.
Your article was well written and we need more coverage on this topic. Please keep writing.
Rosemarie Hughes, Hazleton, Pa
#Readers #tweeters #ways #support #primary #care
Image Source : kffhealthnews.org